Cybersecurity threats to medical devices are a growing concern
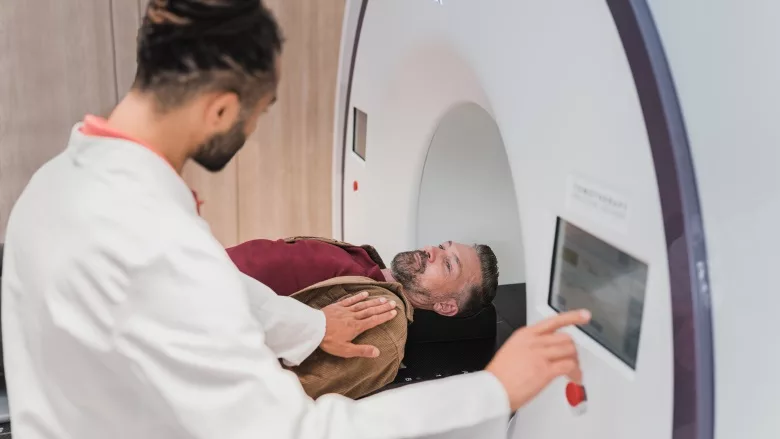
Image via Unsplash
Medical devices include everything from surgically implanted inert pieces of plastic to complex technical IoT systems that are connected to the patient on one side and the network on the other. It is these “connected devices” that everyone, including healthcare leaders, heads of hospital IT and even patients are worried about. This is especially so in times of growing cyber threats and rising geopolitical tensions, with the main perpetrators of international cybercrime: Russia, China, North Korea and Iran.
Connected medical devices include an array of typically large diagnosis machines — CT, X-Ray, PET, MRI, ultrasound; treatment systems such as ventilators, infusion pumps, defibrillators, radiotherapy and chemotherapy devices; and a multitude of systems for patient monitoring and management. They also include a rising use of pharmacy and surgical robotic systems, as well as systems used in the management of hospital buildings, such as HVAC systems which provide hospitals with negative airflow to contain pandemic disease and clean rooms for surgery. These systems also include a wide array of laboratories, CCTV, elevators, door locks and other building systems critical to hospital workflow and safety.
The trouble is that most Health Internet of Thing (HIoT) devices were built with very narrow design parameters, so they lack the hardware capacity to run newer operating systems, as well as the storage to support a patched application if the upgrade increases the size of the application footprint. Many manufacturers refuse to spend money on developing or testing patches or security fixes because that cost was never built into their business model. Instead, they prefer their customers to purchase a newer more secure device, even though there may be many years left on the amortization schedule of the existing system — a device which probably works perfectly fine, aside from the security risks it presents to the medical network and to the safety of patients.
In such cases, hospitals and their clinical engineering and cybersecurity teams are faced with the prospect of retiring devices early, carrying the risk and cost, potentially millions of dollars, of patching these devices outside of manufacturer warranties, or implementing compensating security controls that will pass audit and allow the continued use of these devices till they can be fully written-off. None of these options were, until recently, easy or appealing to healthcare leaders.
Hospitals today have tens of thousands of medical devices connected to their networks. Most are never patched and many contain significant cybersecurity vulnerabilities. The danger is that they could be easily compromised by cyber attackers and used as a foothold to gain access to a network to execute a much greater attack involving the wholesale theft of personal health information or used to launch a ransomware attack or other cyber extortion exercise. The scariest risk, however, is that medical devices could pose a dangerous safety threat to the patients they diagnose, treat, monitor or manage. As such, it is the patient safety concern that troubles most people when discussing this subject.
New devices seeking FDA approval after 2023 will need to be designed with much greater levels of security and patient safety thanks to new FDA rules that arise from the 2022 Patch Act. This will also force manufactures to perform continuous risk analysis of their systems, to release timely patches when vulnerabilities are discovered and to share a Software Bill of Materials (SBoM) with healthcare providers. This will improve the security of new devices. However, the Act doesn’t address the millions of legacy systems that will continue to be used for the next decade or more. Nor does it address the inevitable gap between a vulnerability being discovered, a patch being made and tested or that patch being applied to all at-risk medical devices in a health system. Patch deployment can be a very labor- and time-intensive activity, so this leaves the door open for hackers to exploit weaknesses, just as it does for IT systems that have yet to receive their updates. Patch deployment is also compounded by the fact that medical systems are often in use 24/7, leaving fewer opportunities to take a system out of service for patching.
Together this means that healthcare leaders need to implement an additional security strategy — one that involves the implementation of compensating security controls. These include additional security layers or measures that compensate for an unpatched vulnerability and include “enclaving” or “segmentation” of at-risk devices using software defined networking (SDN) controls built into modern networks. However, before SDN controls can be activated, network security administrators need to “zero trust profile” all medical devices to understand exactly which IP ports, protocols and destination addresses each system needs to communicate with and this is where the difficulty lies.
Fortunately, next generation artificial intelligence (AI)-based tools automate this process through a progression of asset identification, risk analysis, profiling and improved medical device management. This allows a multitude of existing security and network security systems to work together seamlessly through the automation and orchestration of these extra layers of security.
As security risks continue to rise, the need for greater levels of automation in conjunction with smart and intelligent AI-based tools becomes ever more necessary. Given the massive and growing shortage of cybersecurity professionals, the alternatives for manual intervention become more of an impracticality and impossibility.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!




.webp?height=200&t=1642454744&width=200)